
International Cesarean Awareness Month aims to raise awareness and educate people about caesareans. This campaign supports a reduction in the number of caesareans where they are not medically necessary. Caesarean Awareness Month also promotes Vaginal Birth After Caesarean (VBAC) and support for recovery from a caesarean.
The International Cesarean Awareness Network (ICAN) is a non-profit organisation whose mission is to improve maternal-child health by reducing preventable caesareans through education, supporting caesarean recovery, and advocating for vaginal birth after caesarean (VBAC).

What is a Caesarean Birth?
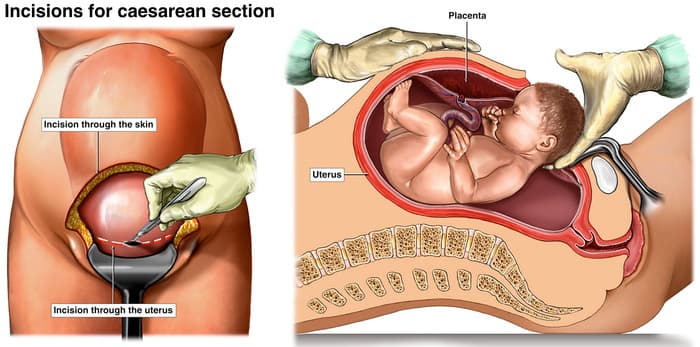
A caesarean section is a major surgical operation in which a baby is delivered through a cut in the front wall of the abdomen and womb. This procedure is often used when a vaginal birth carries a higher risk of complications for the baby and/or the mother, but they can also be elective.
Why might a mother need a Caesarean?
The most common reasons for needing a caesarean are:
- your baby is in the breech position (bottom first) and your doctor doesn’t recommend a vaginal breech birth
- your baby is transverse (lying sideways) and can’t be turned by the doctor
- you have twins and the first one is in the breech position
- your placenta is partly or completely covering the cervix (opening to the womb)
- you have had a previous caesarean
- In an emergency, the baby may need to be delivered very quickly.
Around 1 in 3 babies in Australia are born by caesarean. This is higher than the rate in many other developed countries. This rate is also increasing, both in private and in public hospitals, although you are more likely to have a caesarean in the private sector.
Recovery after a Caesarean
Typically, it takes a lot longer to recover from a Caesarean than it does from a vaginal birth. Firstly, the mother remains in recovery before being taken to the post natal ward, where she will stay in bed until the epidural or spinal anaesthetic wears off. The drip and bladder catheter are usually removed in the first 1 to 2 days. Gentle walking is encouraged to reduce blood clots or the chance of infection. It is important to take things gently after a caesarean. Mum and baby should be able to go home after about 3 to 5 days, with continued rest and recovery.
It’s uncomfortable and somewhat painful to actually function as a Mum whilst recovering after a caesarean, as you are restricted with your movement and limited with how much weight you can pick up. Some people do not understand or appreciate the recovery from a caesarean – you’re expected to just get on with your new life, without acknowledging that you’ve just had major abdominal surgery.
Future Pregnancies
There is a higher risk of future pregnancy complications after a caesarean. It is possible to have a vaginal birth after caesarean section (VBAC). This is a safe choice for most women but there are risks involved. A planned caesarean may be the recommended option for the next birth. The risks of pregnancy complications increase with each caesarean.
Birth Trauma
Unless it is a planned caesarean, no-one talks to you about what might happen if you should need an emergency caesarean. Birth Trauma following an emergency caesarean is very real and should not be ignored because this can lead to post natal depression. This excerpt from the Australasian Birth Trauma Association is a great read for birth trauma after a caesarean:
THE UNEXPECTED EXPERIENCE OF AN EMERGENCY C-SECTION
For many women with uncomplicated pregnancies, a lot of time is spent with their midwife, GP or obstetrician planning for a vaginal delivery. Unfortunately, as part of this planning, discussions about what an emergency C-section is, what it involves and why it may be needed is often not discussed with women. Consequently, an emergency C-section can be an unexpected outcome. In this moment, women go through an experience of a difficult and complicated vaginal birth that results in being rushed into an operating room, and being given a spinal or epidural anaesthesia, and in some cases a general anasthaetic. Women may feel powerless and are unaware of what is occurring to them as doctors are needing to work quickly. As a result, some women can experience emotional trauma in addition to physical trauma following an emergency C-section, including feelings of guilt, failure, disappointment in the healthcare system and disappointment in their body.
Post-traumatic stress disorder (PTSD) is a common experience for women following an emergency C-section, with research suggesting that approximately 1 in 5 women develop PTSD even when the baby is delivered safely.2 If you feel like you are not coping emotionally following an emergency C-section, it is important that you reach out to your support network- friends/family and healthcare workers, including your GP. Signs include:
- Guilt
- Anxiety
- Nightmares
- Difficulty going to or staying asleep
- Social isolation or withdrawing from pleasurable activities
- Hyperarousal
- Intrusive traumatic memories of the event
Melville mums share their stories
We have a couple of amazing mums from the Melville Mums Facebook group who have shared their experiences in the hope that it will raise awareness of the world surrounding caesareans and offer some support for anyone going through recovery.
Planned C-Section
“I’ve had two “planned” caesarians (though both children arrived earlier than scheduled so they were technically classified as “emergency”). I have a chronic health condition that would’ve made childbirth even more difficult than it normally is, so after lots of research and after attending the hospital’s birth classes the decision was made that caesarean would be the best option. I felt much more at ease with what was to come because I felt I’d researched and prepared as much as I could.
With both my bubs my waters broke prior to the scheduled surgery dates so into the hospital we rushed. Both times we got to the hospital within an hour, was hooked up to the monitor to check bubs status and monitor contractions (they came quicker and faster for round two). We then waited for the anaesthetist, obstetrician and paediatrician to arrive before I got wheeled off to theatre, turning on the lights as we went (as both times were after hours). I got moved from the bed to the operating table, a nice warm blanket then the cannula in my hand for the drip. Next I got propped up on the side of the bed for the numbing needle in my back before the spinal tap (which I could barely feel). I did have to pause the anaesthetist multiple times during my second birth though as he was trying to get me to “relax” to put in the needle mid (very painful) contraction (I was not keen on that!). The spinal tap, while not painful, was still what I was hesitant about and my “what was I thinking?” moment, which luckily passed very quickly. The numbing works really quickly so I got laid back down, catheter was put in and ice blocks used to check for feeling. They jiggled the table around to make sure the spinal had worked in all the important areas then the sheet went up to block my view and off they went! It was SO quick; there’s tugging and pulling but no pain, then after what felt both like seconds and an eternity we heard that beautiful, heart warming (tear-jerking) cry from bub. With my second the amazing anaesthetist even dropped the sheet so I could see my girl as she was birthed, before they brought bub around to show us on the other side of the sheet. After a quick health check, my husband cut the umbilical cord then bub was wrapped up and given to me for cuddles while I got stitched up. That probably takes the longest (although realistically not even that long) but I never noticed as baby-effect was always in full force. From water breaking to bub being born was only around three-four hours!
Both times were thankfully standard with no complications (despite my first being born premature at 35+5 and being told that NICU here or even at another hospital might be needed – luckily it wasn’t – and my second at 38 weeks). We were back in the hospital room within an hour or two, feeding and hooked up to (what felt like) a thousand monitoring machines. The next 24 hours were the hardest parts for me; compression equipment on your legs, cannula, catheter, hospital gown and a million cords. Within 24 hours I was walking, majority of cords out and had showered (there is nothing quite like that first post-op shower; bliss). I was lucky to have my husband stay with me both times so he could get up to both bubs and change their nappies, swaddle, etc. and bring them to me.
Recovery was a lot harder the second time as I not only had to look after myself and a newborn, but an energetic toddler as well, so I felt I had no time to recover or “sleep when the baby sleeps” (is that even a thing?), however I knew more about what to expect, so mentally it was easier.
Despite being classed as “emergency” I still had great experiences with both my c-sections as I felt prepared and informed. And I got two beautiful little humans from it <3
Tips
- Research as much as you are comfortable with, but try and cover the main things like what to bring, what the procedure entails (cannula, epidural/spinal, catheter and even the adrenalin shakes after the op) so you feel more prepared should the need for a c-section arise.
- Prep your partner (and even other children) early about what you can and can’t do, like no driving, lifting anything other than your newborn, and vacuuming (which they should for sure start doing during pregnancy to practice).
- Practice getting in and out of bed without using your stomach muscles.
- If you have a date pre-booked still make sure your hospital bag is ready in advance; you can still go early! And make sure your partner knows where everything is so they can bring you what you need (quickly). Your partner is (normally) allowed in the OR with you, so make sure they have closed-in shoes.
- Nurses in the operating room can often take photos on your phone for you if you ask.
- Don’t look at any reflective objects in the OR unless you want to see what’s going on (that includes the roof).
- Ask for, and keep up with, your pain meds (and remind the nurses if they are running behind).
- Don’t over do it! Particularly when you are on pain management it’s easy to think you’re feeling better than you are. You’ve been through major surgery. Most people get put on bed rest after surgery – and you have to look after a tiny human! Ask for (and accept) as much help as you can.
Emergency C-Section
“Our first baby was a planned home water birth through the Community Midwifery Program and with a doula. I am not a fan of hospitals and I get ‘white coat fever’ (my blood pressure goes up in hospitals), so I would be more relaxed at home and it was more comfortable for me to birth in the comfort of our home, as long as everything was medically ok.
My estimated due date came and went, my Braxton hicks kept tricking me into thinking this was it, as you do with your first baby! Then on the Friday I was gardening, I went to the toilet and I lost my mucus plug – great, she’s on her way! Fast forward just over 48 hours of irregular contractions, no sleep, in and out of the birthing pool, then the contractions got so much stronger but still irregular, I had barely dilated and I had reached my limit of trying to birth our first born at home. I spoke to my midwife and decided that I needed help bringing her safely into the world, so off to hospital we went at 10.30pm on the Sunday. I had a cocktail of birthing aids! Methadone (which did nothing), gas, my waters were broken in which they found meconium, then our baby’s heart rate dropped, then we had to go in to theatre for an emergency C-section. Once this was decided, which it all seemed like a blur the next day, my body started to push, but I wasn’t dilated, so it was causing more damage to the baby because I was pushing but there was no where for her to go, so I was told that I wasn’t allowed to push! Can you imagine holding that urge to push when every muscle in your body is telling you to push.
Off to the anaesthetist I went, who had been called in from home, I proceeded to not be very polite to him during his attempt to introduce himself to me, then I was in theatre being prepped to meet my baby. The spinal block worked quickly and all of the pain and pushing went away. My husband was next to me and my midwife was the other side of the cloth waiting to meet me baby. Whilst I couldn’t feel any pain, I could definitely feel tugging and pulling as our little girl was brought earth side. She had fluid on her lungs and got taken away into NICU, I didn’t get to hold my baby. We had shared that intense journey together and we didn’t get to cuddle for what seemed hours and hours. I was taken into recovery where my body shivered until the anaesthetic wore off. I got taken to my recovery room where I waited and waited to hold my baby. She was eventually brought through and we have cuddled every day since.
My recovery from the surgery was hard, tiring and long.
Fast forward 6 months and welcome birth trauma! It hit me that I had no idea what had happened during the surgery, I had no idea of the process, I didn’t get to welcome my baby once she left the comfort of my womb. I thought my body had failed me, failed our baby and that it didn’t do the job it was supposed to do. I was devastated. Then I got the comments “as long as your baby was healthy and safe, that’s all that matters” Well no, in fact it’s not all that matters. I wasn’t ready to deal with the trauma, to process it and to overcome it. I knew I had to wait until I had to deal with it again.
Then came the second pregnancy. I dealt with the birth trauma through support and affirmations, I processed it, I realised that my body didn’t fail me/us, it did exactly what it needed to do, it told me that she needed to come out another way. My planned VBAC was through the Community Midwifery Program again, at King Eddies, with the same doula. He came late also, laboured in hospital with candles, music and oils. I had a nice warm shower, cups of tea. My water’s broke this time, in a big gush! Contractions ramped up, then I could feel that everything started to go in the same direction as the first labour, the pains were in the same place, I had some internal bleeding coming from my uterus, which is a risk of a VBAC and I looked at my midwife and said that if we need to have a C-Section again lets do it. They prepped me for surgery, took me through to theatre, the doctor looked at me and said that I had fully dilated and I could push the baby out. So I did and I got my VBAC! I still needed to recover from the anaesthetic but our son got skin to skin straight away and spent the whole time snuggled with me, and we too have cuddled every day since.
When our first born was about 2 years old she saw my C scar, she asked me what it was and I said that’s a scar from when you were born and she repeated it back to me and said ‘star’. I cried. It was beautiful, she had just turned my caesarean experience into something so special.”
Birth is birth, however your baby enters the world.
Have a look at the Raising Children Network for some great resources on Caesarean births and recovery. If you or anyone you know need help with Perinatal Mental Health, you can find some great information and inspirational stories in our blog Breaking Down Barriers.